Automation is Key to Billing Smarter, Not Harder
The more you automate and use best practices for medical billing, the better chance you have of helping your clients to get paid quickly and correctly.
By Cher Knebel

With so much going on in the world today, having to spend more time than necessary to complete routine tasks in your billing agency is simply not “working smart.” The key to maximum efficiency and productivity is through automation. The more you automate and use best practices for medical billing, the better chance you have of helping your clients to get paid quickly and correctly. Not only does minimizing delays and denials in the claims process positively impact your clients, but it also makes a difference for providers, patients, and general public health.
How does automation help? An automated system is composed of elements designed to perform a set of tasks that have been programmed. Operational and repetitive tasks become less of a burden and makes the workday simpler and easier for you and your staff. The best-case scenario is finding a solution that can automate billing from end to end, eliminating as many places where errors occur as possible.
Cost and Time Savings With Automation
According to the Medical Group Management Association (MGMA), when a claim is denied—often because of a manual error—the cost to rework is $25. With the average cost to process an initial claim at $6.50, that is a total cost of $31.50 when a claim is denied. With billing software, there are multiple billing tasks that you can automate and stop doing manually, which can add up to thousands of dollars in labor savings from not having to make related calls, investigative work, or appeals.
By utilizing an electronic charge capture process and claims submission software to scrub 100% throughout the entire claim process, you are able to capture and submit the day the superbill is received to reduce coding errors, prevent over and under coding, improve accuracy, and decrease data entry for the billing staff. Your goal should be to get claims submitted in three days or less from the time of service, then track them through payment.
Moreover, billing features like no-response claim tracking can also help ensure that no claim goes unpaid or underpaid. To ensure accurate payments, keep fee schedules up to date and use electronic remittance advice to post payments in a practice management system. Underpayments result in a 7% loss of net revenue for your average practice client, but it doesn’t have to happen to yours. When all your billing practices are automated and in order, you should be able to achieve average days in A/R of 40 days or less and have a net collection rate of 96%.
In addition to improved accuracy, automation helps to minimize the number of staff needed to do client claims processing. It also helps unify payment data from multiple channels, including collection procedures, debit transactions, and paper checks.
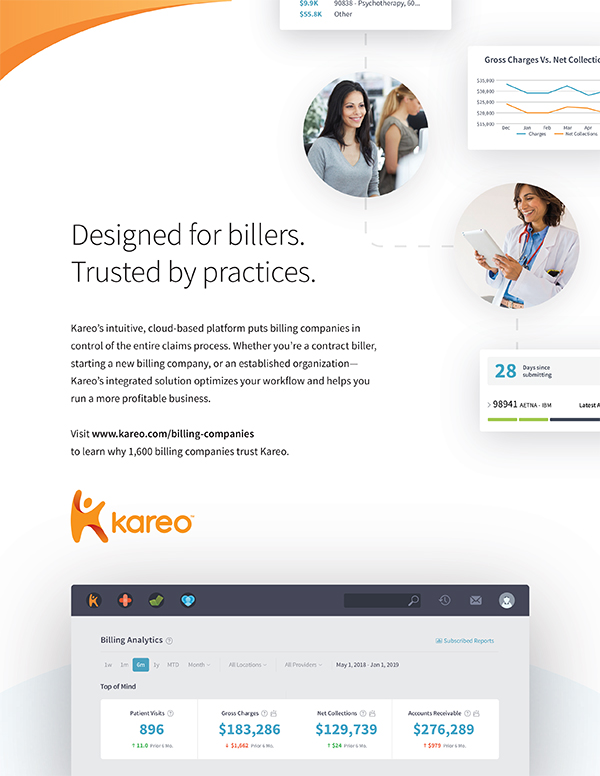
Advertisement. Click on image to visit advertiser's website. Story continues below.
|
Automation Mistakes to Avoid
Once you have decided to go with full automation of your billing tasks and have chosen a billing software vendor to partner with—or change to—here are a few mistakes to avoid so you can get the maximum output from your billing software:
- Not understanding the full function of your system.
Every system is different, and it often takes a little time and patience to make it work best for both your company’s and clients’ needs. Be sure your staff takes advantage of all training available from the vendor. Conduct follow-up training meetings to discuss any difficulties the staff is experiencing with the software—this could be an opportunity for knowledge share as well as “lunch and learns” for your staff. You may also want to consider retraining at the six-month mark to see if everyone is utilizing everything in the system. It’s difficult to absorb all aspects of a system, especially one with advanced functionality, during the initial training.
- Missing tasks that can be automated.
It’s important to know what new applications of technology are available in your software. Especially when your client transactions increase as reimbursement amounts decrease, you need automation to maintain profitability for your billing company. Successful billing companies recognize that their software helps them to do more work with fewer people, and every billing task should be considered for automation. If your software vendor has a newsletter or regular product updates, be sure to subscribe and read them to stay abreast on new functions and technology as they become available.
- Batching work.
When things get especially busy, it is easy for billing staff to batch tasks and put them aside to avoid using the new automation processes. But where batching does work is when a staff person batches similar tasks that work with the automated processes. A person gains momentum doing the same task repeatedly—finishing the job faster than going back and forth with completing different types of tasks.
- Automation is only as good as the staff that uses it.
Be sure to have a mechanism in place to check that the staff is using the technology properly, and establish key milestones to track how your company is benefiting.
Helping your clients get paid continues to be more challenging with each passing year. While it may require a little time up front to get used to new processes, using automation to complete your many billing tasks will help make a big difference in the accuracy and amount you can collect on behalf of your valued clients.

Cher Knebel is a senior content marketing manager at Kareo and joined the company in 2019. She has been a content creator for more than two decades, specifically working in healthcare communications for 15 years. In previous communication roles, Knebel worked in a variety of industries, including technology, managed care, public utilities, and as a freelance writer for small businesses and local publications. Her most recent role was communications manager in the health benefits industry.
For additional information to help your billing practice, visit Kareo.com/resource-library and click on “Billing” in the content category.
|