We asked the following questions and received the following responses:
Question 1
What Is Your Denial Percentage? (25 responses)
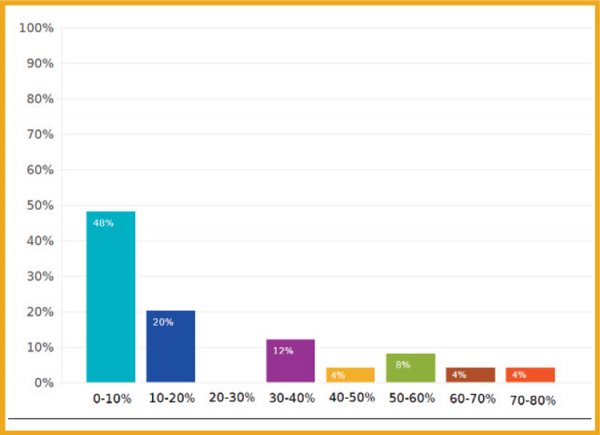
Answers were selected from dropdown ranges, i.e. 0-10%, 10-20%, etc. The chart above represents the percentage of respondents who selected that denial range, i.e. just under half the respondents (48%) said their denial rate was in the single digits.
Question 2
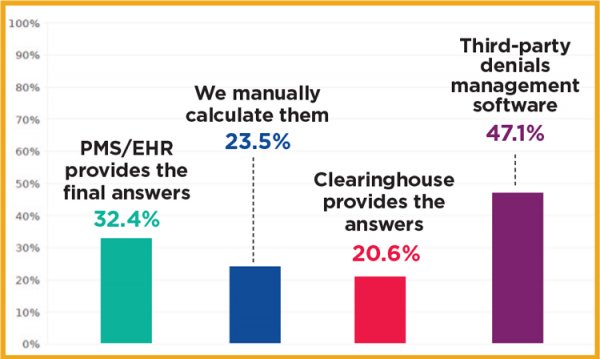
How Do You Calculate Your Denial Rate? (34 responses)
Question 3
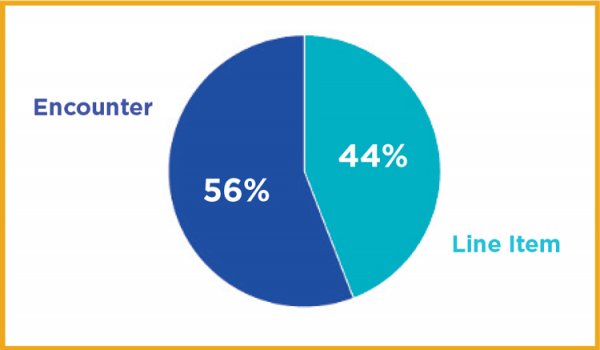
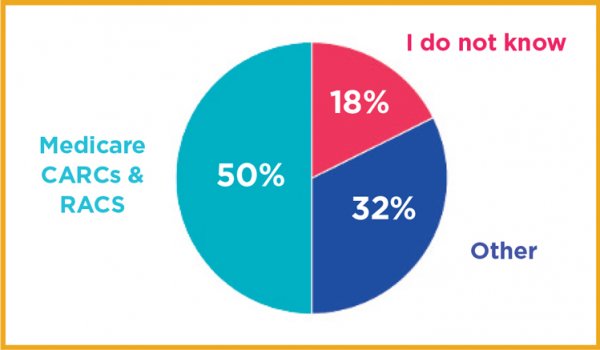
What Definition Are You Using? (34 responses)
Question 4
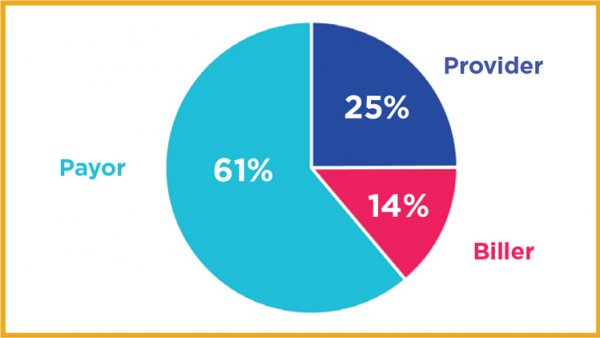
What Percentage of Denials Do You Attribute to the Payor, Biller, or Provider? (32 responses)
Note: For the purpose of averaging, we eliminated responses that did not total 100%, as it appears some respondents interpreted the question as what the denial rate was when grouped for each of the parties.
Question 5
What Are Your Top 5 Denial Codes? (32 responses)
#1 Code: 109
Claim/service not covered by this payer/contractor. You must send the claim/service to the correct payer/contractor.
#2 Code: 16
Claim/service lacks information or has submission/billing error(s). Usage: Do not use this code for claims attachment(s)/ other documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
#3 Code: 197
Precertification/authorization/notification/pre-treatment absent.
#4 Code: 97
The benefit for this service is included in the payment/ allowance for another service/procedure that has already been adjudicated. Usage: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
#5 Code: 50
These are non-covered services because this is not deemed a ‘medical necessity’ by the payer. Usage: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
#6 Code: 22
This care may be covered by another payer per coordination of benefits.
Question 6
What Are Your Top Denial Reasons? (31 responses)
For simplicity, we have ranked them in descending order by the percentage of respondents who listed it as their top reason.
#1: Incorrect/Additional Information Required 27.6%
#2: Eligibility/Benefits 27.6%
#3: Coding (including Bundling, Payor Policies, etc.) 17.2%
#4: Credentialing/Contracting 13.8%
#5: Other 10.5%
#6: Medical Necessity 7.1%
#7: Authorization 3.9%
#8: Billing Error 3.6%
Question 7
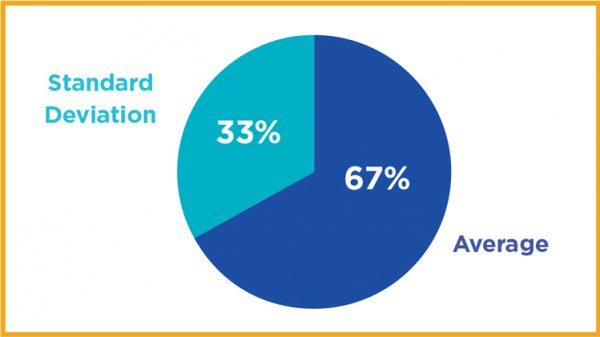
What Percentage of Your Denials Are Overturned and Paid Upon Resubmission and Appeal? (28 responses)
Question 8
How Are You Calculating the Denial Rates for This Survey? (34 responses)